 |
October-December 2012
Volume 6 | Issue 4
Page Nos. 101-137
Online since Friday, January 18, 2013
Accessed 18,585 times.
PDF access policy
Full text access is free in HTML pages; however the journal allows PDF access only to users from SOUTH AFRICA and paid subscribers.
EPub access policy
Full text in EPub is free except for the current issue. Access to the latest issue is reserved only for the paid subscribers.
|
| |
|
|
Show all abstracts Show selected abstracts Add to my list |
|
| ORIGINAL ARTICLES |
|
|
  |
Muscle activation patterns in patients with recurrent shoulder instability |
p. 101 |
Anju Jaggi, Ali Noorani, Alex Malone, Joseph Cowan, Simon Lambert, Ian Bayley
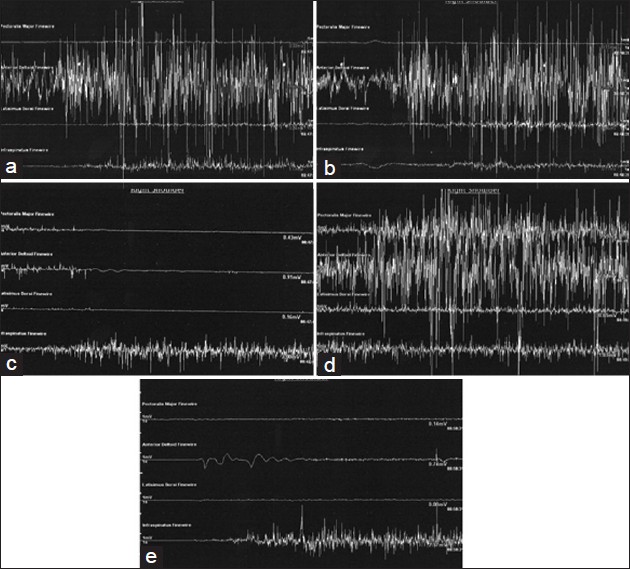
DOI:10.4103/0973-6042.106221 PMID:23493512Purpose: The aim of this study is to present muscle patterns observed with the direction of instability in a series of patients presenting with recurrent shoulder instability.
Materials and Methods: A retrospective review was carried out on shoulder instability cases referred for fine wire dynamic electromyography (DEMG) studies at a specialist upper limb centre between 1981 and 2003. An experienced consultant clinical neurophysiologist performed dual needle insertion into four muscles (pectoralis major (PM), latissimus dorsi (LD), anterior deltoid (AD) and infraspinatus (IS)) in shoulders that were suspected to have increased or suppressed activation of muscles that could be contributing to the instability. Raw EMG signals were obtained while subjects performed simple uniplanar movements of the shoulder. The presence or absence of muscle activation was noted and compared to clinical diagnosis and direction of instability.
Results: A total of 140 (26.6%) shoulders were referred for fine wire EMG, and 131 studies were completed. Of the shoulders tested, 122 shoulders (93%) were identified as having abnormal patterns and nine had normal patterns. PM was found to be more active in 60% of shoulders presenting with anterior instability. LD was found to be more active in 81% of shoulders with anterior instability and 80% with posterior instability. AD was found to be more active in 22% of shoulders with anterior instability and 18% with posterior instability. IS was found to be inappropriately inactive in only 3% of shoulders with anterior instability but in 25% with posterior instability. Clinical assessment identified 93% of cases suspected to have muscle patterning, but the specificity of the clinical assessment was only correct in 11% of cases.
Conclusion: The DEMG results suggest that increased activation of LD may play a role in both anterior and posterior shoulder instability; increased activation of PM may play a role in anterior instability. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
Symptomatic chronic long head of biceps rupture: Surgical results |
p. 108 |
Chye Yew Ng, Lennard Funk
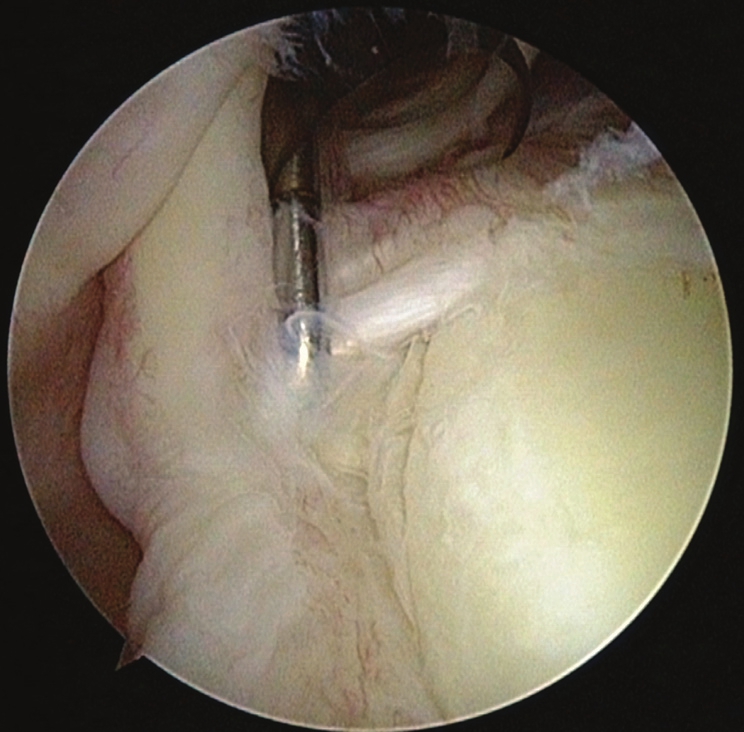
DOI:10.4103/0973-6042.106222 PMID:23493581Purpose: Chronic rupture of the long head of biceps (LHB) tendon is usually asymptomatic. However, some active patients suffer with long-term cramping pain associated with repetitive biceps use. The aim of this study is to review the outcomes of biceps tenodesis performed for chronic LHB ruptures.
Materials and Methods: We performed a retrospective review of 11 consecutive patients who underwent biceps tenodesis for symptomatic chronic LHB ruptures over a 4-year period.
Results: There were 10 men and one woman with an average age at surgery of 41 years (range 23-65). The mean follow-up was 29 months (range 6-60). In five cases a tendon was still identifiable and suitable for repair with an 'in-bone' interference screw. However, in six cases the tendon was not possible to tenodese with an interference screw. In these cases we used an 'on-bone' technique with suture anchors. All, except one, patients reported improvement in their arm pain (78%), strength (74%) and appearance. All, except one, were glad to have had the surgery.
Conclusions: Symptomatic chronic LHB ruptures improve with a biceps tenodesis procedure. Due to the chronicity of the injury and possible degeneration of the tendon, a suitable tendon for 'in-bone' tenodesis may not be possible. In these cases an 'on-bone' footprint repair with suture anchors achieves good results.
Level of Evidence: IV (retrospective case series). |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (2) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Does age or gender of the patient influence the outcome of type II superior labrum anterior and posterior repair? |
p. 112 |
Daniel Mok, Emily L Wang
DOI:10.4103/0973-6042.106223 PMID:23493640Aims: To assess whether patients above 50 years of age, particularly female, would benefit from repair of their SLAP tears.
Settings and Design: Review of patients' records followed by telephone interview at a minimum of two years after surgery.
Materials and Methods: Seventy-two consecutive patients who had their SLAP repaired were retrospective reviewed by an independent examiner. Follow up was by telephone interview with pain and functional results measured according to the Oxford Shoulder Questionnaire. The patients were asked whether they would undergo the same operation if they had a similar injury.
Statistical Analysis Used: OKS - One way ANOVA, followed by Tukey HSD multiple comparisons were used to assess the Oxford Shoulder score. Kruskal-Wallis Test was used to assess the final VAS Pain Score. Student's T tests for Oxford scores before and after surgery.
Results: Between 2007-2008, 38 male patients and 34 female patients with an average age of 53 (19-75) years had their SLAP repair. Good to excellent results in Oxford shoulder scores were reported in 94%. 68 0f 72 patients would undergo the same if they had a similar injury. No statistical correlation was found between the patient's age, gender and outcome scores.
Conclusions: Neither the patients' gender nor their age above 50 affected the outcome after surgery. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
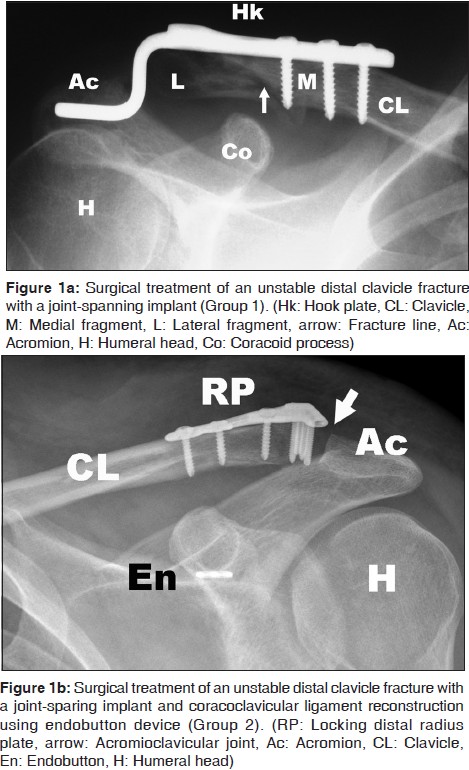  |
Surgical treatment of lateral clavicle fractures associated with complete coracoclavicular ligament disruption: Clinico-radiological outcomes of acromioclavicular joint sparing and spanning implants |
p. 116 |
Deepak N Bhatia, Richard S Page
DOI:10.4103/0973-6042.106224 PMID:23493665Purpose: Distal clavicle fracture associated with complete coracoclavicular ligament disruption represents an unstable injury, and osteosynthesis is recommended. This study was performed (1) to retrospectively analyse the clinico-radiological outcomes of two internal fixation techniques, and (2) to identify and analyse radiographic fracture patterns of fracture that are associated with this injury.
Materials and Methods: A total of 15 patients underwent osteosynthesis with either (1) acromioclavicular joint-spanning implants (Group 1, Hook plate device, n = 10) or (2) joint-sparing implants (Group 2, distal radius plate, n = 5); these were reviewed at a mean period of 26.1 months (12 to 40 months). Clinical outcomes were measured using Constant Score (CS), Simple Shoulder Test (SST), and Walch ACJ score (WS). Radiographs and ultrasonography were used to assess the glenohumeral and acromioclavicular joints, and the subacromial space. Preoperative radiographs were analyzed for assessment of fracture lines to identify radiographic patterns. Statistical analysis of the data was performed to determine any significant differences between the two groups.
Results: The overall clinical outcome was satisfactory (CS 80.8, SST 11.3, WS 17.6) and a high union rate (93.3%) was observed. Radiographic complications (acromioclavicular degeneration and subluxation, hook migration, abnormal ossification) did not negatively influence the final clinical outcomes. Four distinct radiographic fracture patterns were observed. A statistically significant difference ( P < 0.05) was observed in the reoperation rates between the two groups.
Conclusions: Internal fixation of this fracture pattern is associated with a high union rate and favorable clinical outcomes with both techniques. A combination of distal radius plate and ligament reconstruction device resulted in stable fixation and significantly lower reoperation rates, and should be used when fracture geometry permits (Types 1 and 2).
Design: Retrospective review of a consecutive clinical case series.
Setting: Level 1 academic trauma service, Public Hospital. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| CASE REPORTS |
 |
|
|
  |
Septic failure is not a septic loosening: A case report of a failed shoulder prosthesis |
p. 121 |
Yde Engelsma, Pieter Buma, Pieter C Geervliet, Arthur Van Noort
DOI:10.4103/0973-6042.106225 PMID:23493778Septic failure of a shoulder arthroplasty due to a low-grade infection is generally called septic loosening. However, it is often not investigated if a prosthesis is genuinely loose. We present a case of a failed resurfacing prosthesis in a 70-year-old woman. This prosthesis failed due to a low-grade infection and a revision procedure was mandatory. All intraoperative cultures were positive and revealed a combination of bacteria. Nevertheless, histology revealed a macroscopic and a microscopic stable prosthesis with full osseointegration beneath the prosthesis. The general conception is that an infection leads to interface formation (with neutrophils) and loosening of the prosthesis. We debate this with the presentation of this case of a failed shoulder prosthesis and we think that periprosthetic infection and septic prosthetic loosening are two different entities. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
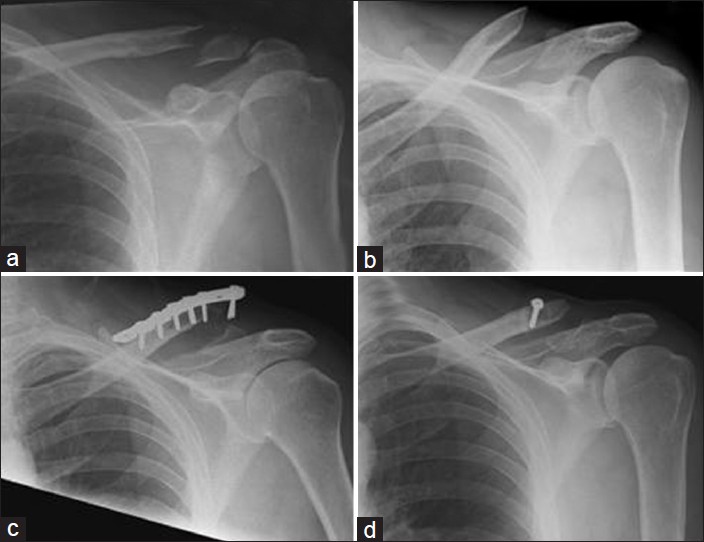  |
Locking plates for displaced fractures of the lateral end of clavicle: Potential pitfalls |
p. 126 |
Soha Sajid, Ross Fawdington, Maneesh Sinha
DOI:10.4103/0973-6042.106226 PMID:23493822Roughly a quarter of all clavicle fractures occur at the lateral end. Displaced fractures of the lateral clavicle have a higher rate of nonunion. The management of fractures of the lateral clavicle remains controversial. Open reduction internal fixation with a superiorly placed locking plate is a recently developed technique. However, there are no randomized controlled trials to evaluate the efficacy of this procedure. We present a series of four cases which highlight the technical drawbacks with this method of fixation for lateral clavicle fractures. Two cases show that failure of the plate to negate the displacing forces at the fracture site can lead to plate pullout. Two cases illustrate an unusual complication of an iatrogenic injury to the acromioclavicular joint capsule which led to joint instability and dislocation. We advise caution in using this method of fixation. Recent studies have described the success of lateral clavicle locking plate fixation augmented with a coracoclavicular sling. This augmentation accounts for the displacing forces at the fracture site. We would recommend that when performing lateral clavicle locking plate fixation, it should be reinforced with a coracoclavicular sling to prevent plate failure by lateral screw pullout. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (3) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| TECHNICAL TIP |
 |
|
|
  |
Improved clinical utility in clavicle fracture decision-making with true orthogonal radiographs |
p. 130 |
Joshua D Harris, James C Latshaw
DOI:10.4103/0973-6042.106227 PMID:23493846Operative treatment of displaced clavicle fractures has demonstrated lower rates of nonunion and symptomatic malunion, improved functional outcomes, and earlier return to activities versus nonoperative treatment. Surgical treatment may offer a reduction in the relative risk of nonunion and symptomatic malunion and an earlier return to work or sport. To present an easy and safe method of acquiring orthogonal views of the clavicle without any manipulation of the patient's upper extremity. Academic medical center and private clinic in the Midwestern United States; retrospective patient cohort. We reviewed records of patients with acute clavicle fractures between January 2010 and August 2011. Thirty-four patients were treated with sling immobilization and 52 patients were treated surgically with superior plate and screw internal fixation. Prior to the introduction of orthogonal views, 19 patients were treated nonoperatively and 22 treated with internal fixation. Addition of orthogonal views increased the number of patients treated surgically: In the same period, 15 patients were treated nonoperatively and 30 with internal fixation. Following surgery, patients were evaluated in the outpatient office at 2 and 6 weeks and 3 and 6 months. Nonoperatively treated patients were evaluated at 1, 2, and 4 weeks and 3 and 6 months postinjury. Standard use of orthogonal views has led to greater utilization of surgical treatment of clavicle fractures at our institution and improved both the understanding and treatment of these injuries. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| LETTERS TO THE EDITOR |
 |
|
|
  |
A peculiar periprosthetic humeral fracture managed in a simple but effective way |
p. 135 |
Abdelsalam Eid, Tarek A Elhewala
DOI:10.4103/0973-6042.106228 PMID:23495285 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
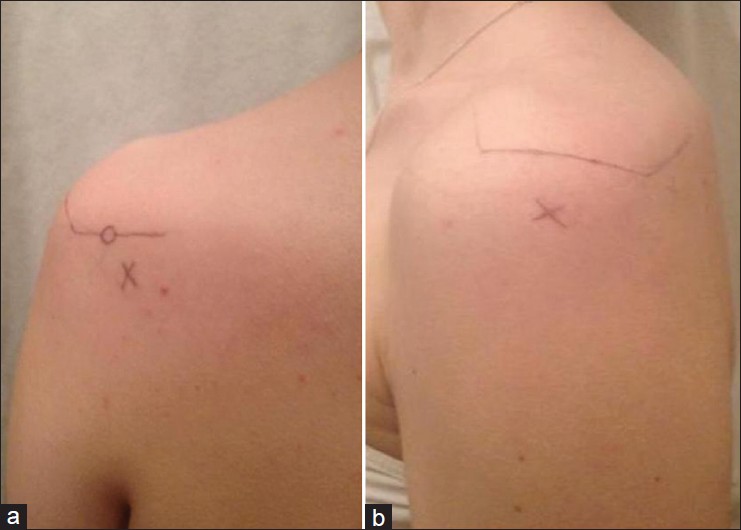  |
Subacromial corticosteroid injection using the posterior or lateral shoulder portals |
p. 136 |
Neil R Wickramasinghe, Nicholas D Clement, Daniel E Porter
DOI:10.4103/0973-6042.106229 PMID:23495286 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
