 |
January-March 2016
Volume 10 | Issue 1
Page Nos. 1-54
Online since Wednesday, January 20, 2016
Accessed 15,396 times.
PDF access policy
Full text access is free in HTML pages; however the journal allows PDF access only to users from SOUTH AFRICA and paid subscribers.
EPub access policy
Full text in EPub is free except for the current issue. Access to the latest issue is reserved only for the paid subscribers.
|
| |
|
|
Show all abstracts Show selected abstracts Add to my list |
|
| EDITORIAL |
|
|
  |
Shoulder, elbow, and wrist: Broadening the scope, and the editorial board |
p. 1 |
Deepak N Bhatia, Joe F de Beer
DOI:10.4103/0973-6042.174510 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| ORIGINAL ARTICLES |
 |
|
|
  |
Midterm clinical outcomes following arthroscopic transosseous rotator cuff repair  |
p. 3 |
Brody A Flanagin, Raffaele Garofalo, Eddie Y Lo, LeeAnne Feher, Alessandro Castagna, Huanying Qin, Sumant G Krishnan
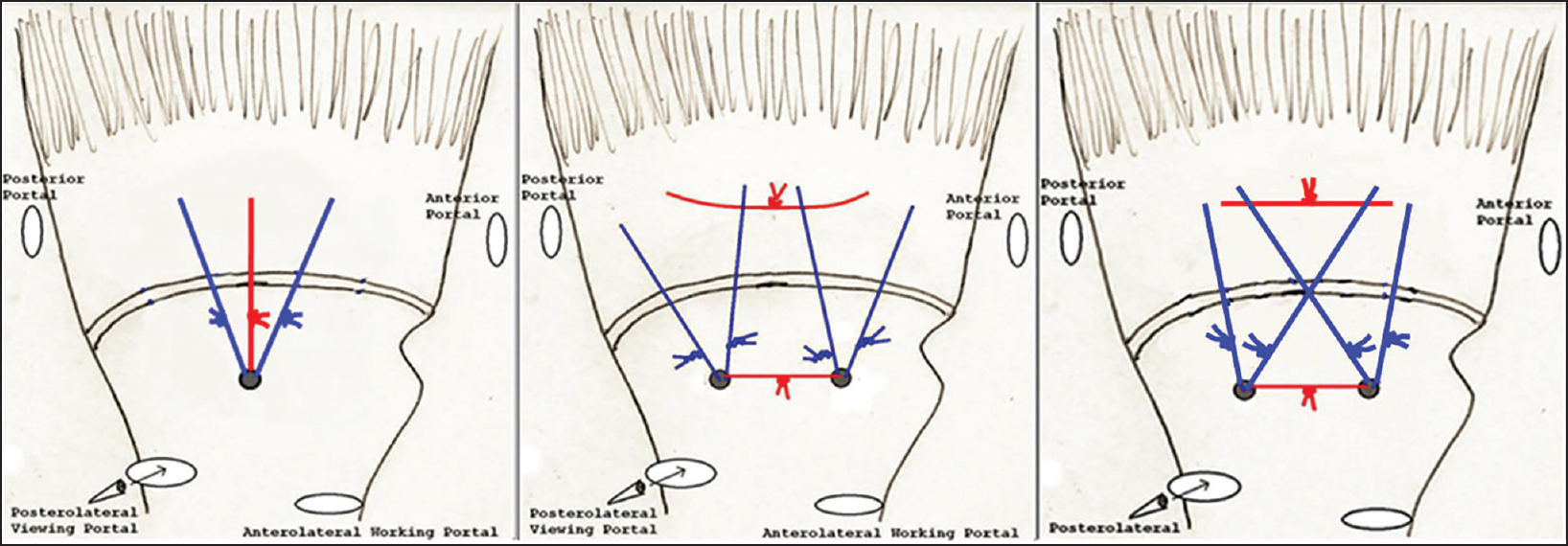
DOI:10.4103/0973-6042.174511 PMID:26980983Purpose: Arthroscopic transosseous (TO) rotator cuff repair has recently emerged as a new option for surgical treatment of symptomatic rotator cuff tears. Limited data is available regarding outcomes using this technique. This study evaluated midterm clinical outcomes following a novel arthroscopic TO (anchorless) rotator cuff repair technique.
Materials and Methods: A consecutive series of 107 patients and 109 shoulders underwent arthroscopic TO (anchorless) rotator cuff repair for a symptomatic full-thickness tear. Pre and postoperative range of motion (ROM) was compared at an average of 11.8 months. Postoperative outcome scores were obtained at an average of 38.0 months. Statistical analysis was performed to compare pre and postoperative ROM data. Univariate analysis was performed using Student's t-test to compare the effect of other clinical characteristics on final outcome.
Results: Statistically significant improvements were noted in forward flexion, external rotation and internal rotation (P < 0.0001). Average postoperative subjective shoulder value was 93.7, simple shoulder test 11.6, and American Shoulder and Elbow Surgeons (ASES) score 94.6. According to ASES scores, results for the 109 shoulders available for final follow-up were excellent in 95 (87.1%), good in 8 (7.3%), fair in 3 (2.8%), and poor in 3 (2.8%). There was no difference in ROM or outcome scores in patients who underwent a concomitant biceps procedure (tenodesis or tenotomy) compared with those who did not. Furthermore, there was no significant difference in outcome between patients who underwent either biceps tenodesis or tenotomy. Age, history of "injury" preceding the onset of pain, tear size, number of TO tunnels required to perform the repair, and presence of fatty infiltration did not correlate with postoperative ROM or subjective outcome measures at final follow-up. Two complications and four failures were noted.
Conclusions: Arthroscopic TO rotator cuff repair technique leads to statistically significant midterm improvement in ROM and satisfactory midterm subjective outcome scores with low complication/failure rates in patients with average medium-sized rotator cuff tears with minimal fatty infiltration. Further work is required to evaluate radiographic healing rates with this technique and to compare outcomes following suture anchor repair.
Level of Evidence: Level IV
|
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
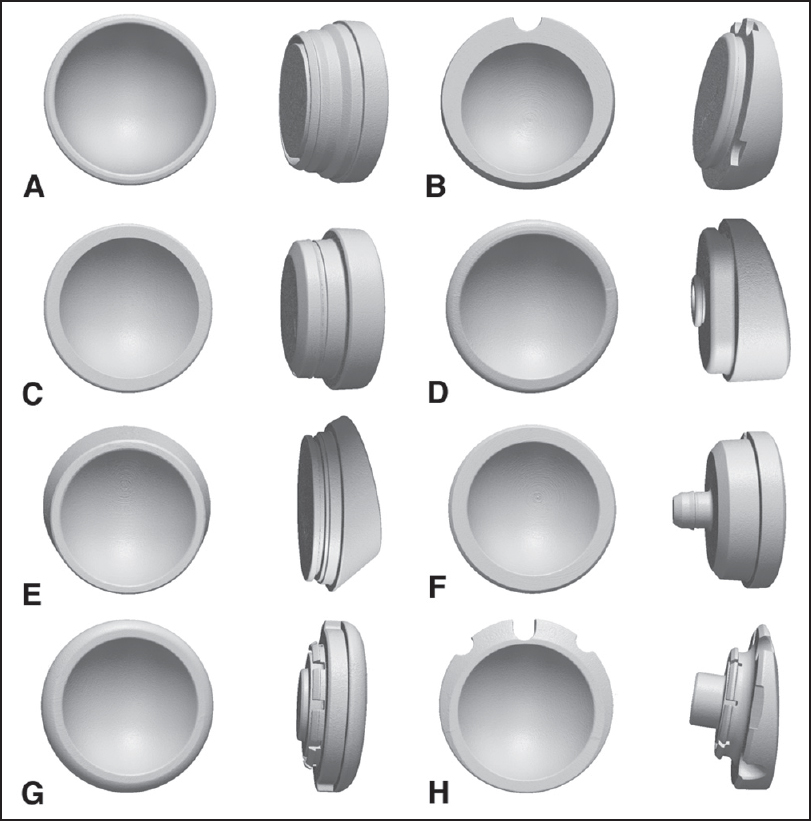  |
Inter and intra-system size variability of reverse shoulder arthroplasty polyethylene inserts |
p. 10 |
Matthew G Teeter, Matthew T Dawson, George S Athwal
DOI:10.4103/0973-6042.174512 PMID:26980984Background: As the incidence of reverse shoulder arthroplasty (RSA) increases, so will the revision burden. At times, the revision surgeon may be faced with a well-fixed component on one side of the joint and revision implants from a different manufacturer. The ability to use glenoid and humeral implants from different manufacturers could simplify the revision procedure. This study hypothesized that across a range of RSA systems, some implants would demonstrate high size compatibility and others would demonstrate low compatibility.
Materials and Methods: Six polyethylene inserts each from eight reverse total shoulder arthroplasty systems were examined (48 total inserts). All inserts were scanned using a laboratory micro-computed tomography scanner at 50 μm isotropic voxel spacing, and their surface geometries were reconstructed. The different implant geometries were co-registered, and the three-dimensional (3D) variability between the articular surfaces of the different implant systems was measured. Intrasystem manufacturing variability was also determined by measuring the 3D variability of inserts from the same system.
Results: The intersystem polyethylene articular surface deviations between same-size systems were not significantly different (P = 0.61) and were a mean maximum of 60 ± 16 μm (range: 30-80 μm). Intrasystem manufacturing variability was equivalent between all but two models, averaging 49 ± 17 μm (range: 23-99 μm).
Discussion: Differences in articular geometry between same-size inserts from different systems were on the same scale as intrasystem manufacturing variability, suggesting that different implant systems of the same nominal diameter could potentially be used interchangeably in revision or extenuating circumstances.
Conclusion: The results of this study suggest that surgeons can theoretically interchange same-sized implant components from the different RSA systems tested when conducting revisions. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
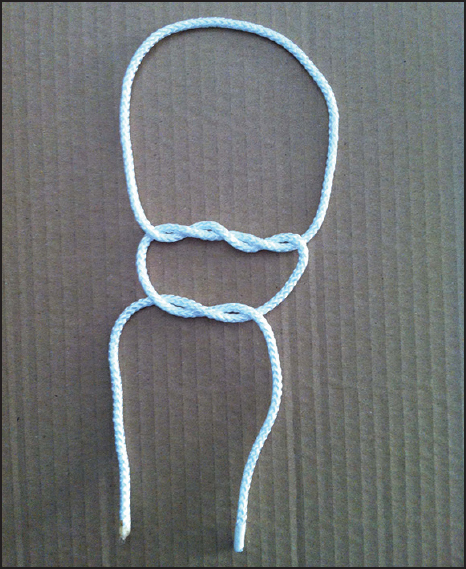  |
Biomechanical evaluation of the Nice knot |
p. 15 |
Shannon W Hill, Christopher R Chapman, Samer Adeeb, Kajsa Duke, Lauren Beaupre, Martin J Bouliane
DOI:10.4103/0973-6042.174513 PMID:26980985Background: The Nice knot is a bulky double-stranded knot. Biomechanical data supporting its use as well as the number of half hitches required to ensure knot security is lacking.
Materials and Methods: Nice knots with, one, two, or three half-hitches were compared with the surgeon's and Tennessee slider knots with three half hitches. Each knot was tied 10 times around a fixed diameter using four different sutures: FiberWire (Arthrex, Naples, FL), Ultrabraid (Smith and Nephew, Andover, MA), Hi-Fi (ConMed Linvatec, Largo, FL) and Force Fiber (Teleflex Medical OEM, Gurnee, IL). Cyclic testing was performed for 10 min between 10N and 45N, resulting in approximately 1000 cycles. Displacement from an initial 10N load was recorded. Knots surviving cyclic testing were subjected to a load to failure test at a rate of 60 mm/min. Load at clinical failure: 3 mm slippage or opening of the suture loop was recorded. Bulk, mode of ultimate failure, opening of the loop past clinical failure, was also recorded.
Results: During cyclic testing, the Nice knots with one or more half-hitches performed the best, slipping significantly less than the surgeon's and Tennessee Slider (P < 0.002). After one half-hitch, the addition of half-hitches did not significantly improve Nice knot performance during cyclic testing (P > 0.06). The addition of half-hitches improved the strength of the Nice knot during the force to failure test, however after two half-hitches, increase of strength was not significant (P = 0.59). While FiberWire was the most bulky of the sutures tested, it also performed the best, slipping the least.
Conclusion: The Nice knot, especially using FiberWire, is biomechanically superior to the surgeon's and Tennessee slider knots. Two half hitches are recommended to ensure adequate knot security.
The level of Evidence: 2, prospective comparative study.
|
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
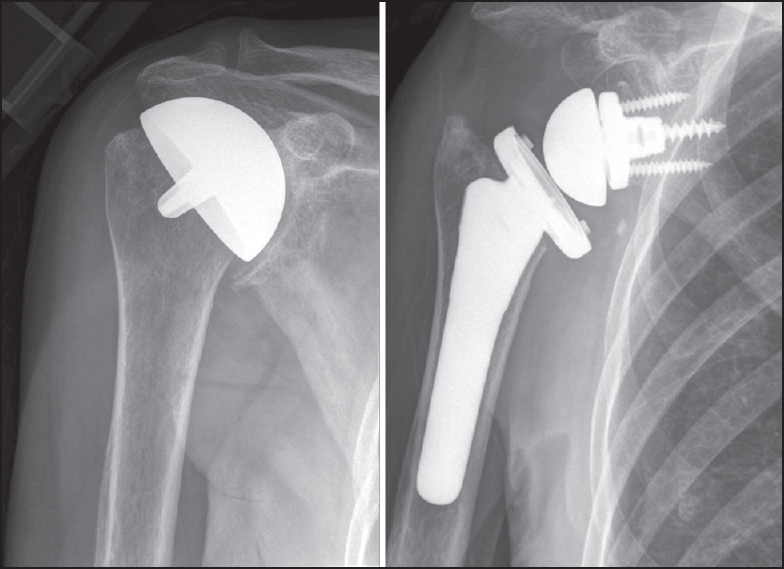  |
Revision of failed humeral head resurfacing arthroplasty |
p. 21 |
Philipp N Streubel, Juan P Simone, Robert H Cofield, John W Sperling
DOI:10.4103/0973-6042.174514 PMID:26980986Purpose: The purpose of this study is to assess the outcomes of a consecutive series of patients who underwent revision surgery after humeral head resurfacing (HHR). Our joint registry was queried for all patients who underwent revision arthroplasty for failed HHR at our institution from 2005 to 2010. Eleven consecutive patients (average age 54 years; range 38-69 years) that underwent revision of 11 resurfacing arthroplasties were identified. The primary indication for resurfacing had been osteoarthritis in six, glenoid dysplasia in two, a chondral lesion in two, and postinstability arthropathy in one patient. The indication for revision was pain in 10 and infection in one patient. Seven patients had undergone an average of 1.9 surgeries prior to resurfacing (range 1-3).
Materials and Methods: All patients were revised to stemmed arthroplasties, including one hemiarthroplasty, two reverse, and eight anatomic total shoulder arthroplasties at a mean 33 months after primary resurfacing (range 10-131 months). A deltopectoral approach was used in seven patients; four patients required an anteromedial approach due to severe scarring. Subscapularis attenuation was found in four cases, two of which required reverse total shoulder arthroplasty. Bone grafting was required in one glenoid and three humeri.
Results: At a mean follow-up of 3.5 years (range 1.6-6.9 years), modified Neer score was rated as satisfactory in five patients and unsatisfactory in six. Abduction and external rotation improved from 73° to 88° (P = 0.32) and from 23° to 32° (P = 0.28) respectively. Reoperation was required in two patients, including one hematoma and one revision for instability.
Conclusion: Outcomes of revision of HHR arthroplasty in this cohort did not improve upon those reported for revision of stemmed humeral implants. A comparative study would be required to allow for definitive conclusions to be made. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| REVIEW ARTICLE |
 |
|
|
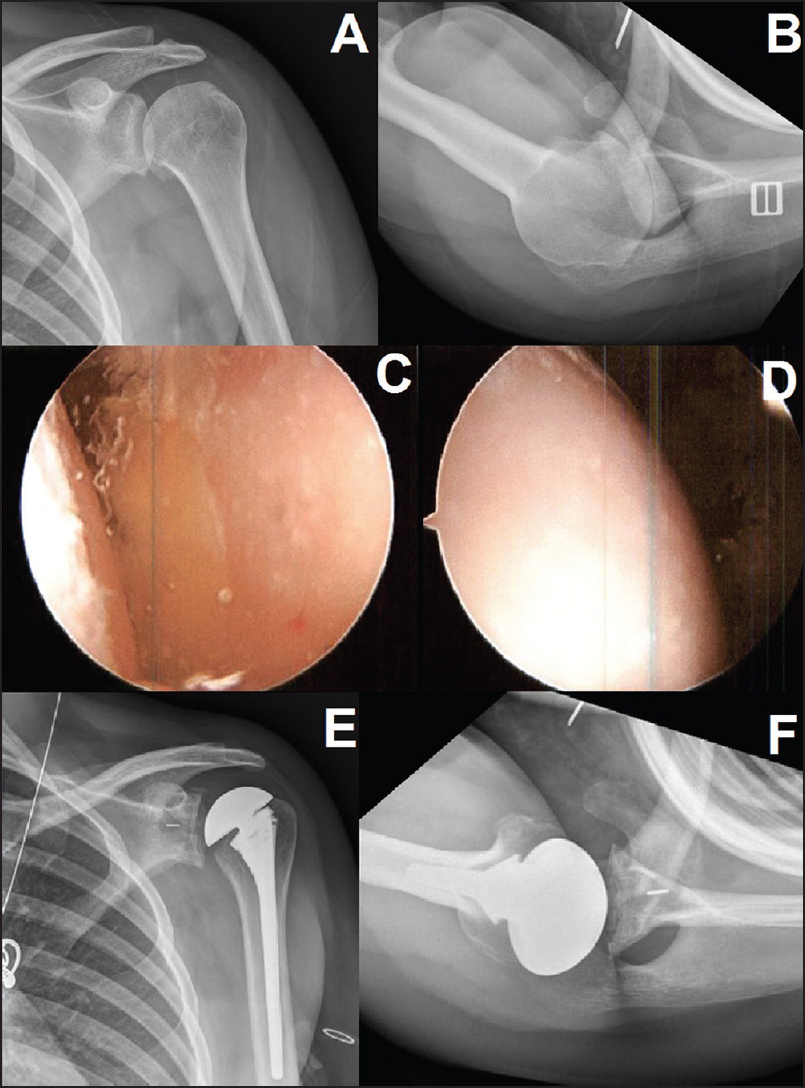  |
Surgical options for the young patient with glenohumeral arthritis |
p. 28 |
Jonathan D Barlow, Joseph Abboud
DOI:10.4103/0973-6042.174516 PMID:26980987Young patients with glenohumeral arthritis are an ongoing treatment challenge. They typically have high demands of their shoulders, require long-term durability due to their young age, and often have altered local anatomy, through their disease process (instability arthropathy, juvenile rheumatoid arthritis, etc.) or from previous surgery (capsulorraphy arthropathy, chondrolysis, etc.). Workup to evaluate underlying causes of early arthritis, and to exclude infectious causes are necessary. When nonoperative management fails, arthroscopic debridement, hemiarthroplasty (isolated, with glenoid reaming, or with biological interposition), and total shoulder arthroplasty are treatment options available to the treating surgeon. Debridement or hemiarthroplasty can provide pain relief for a subset of patients, but results have not been reproducible across the literature and have not been durable over time. Total shoulder arthroplasty provides the most reliable pain relief, but long-term glenoid loosening and wear continue to lead to high revision rates in this patient population.
|
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| CASE REPORTS |
 |
|
|
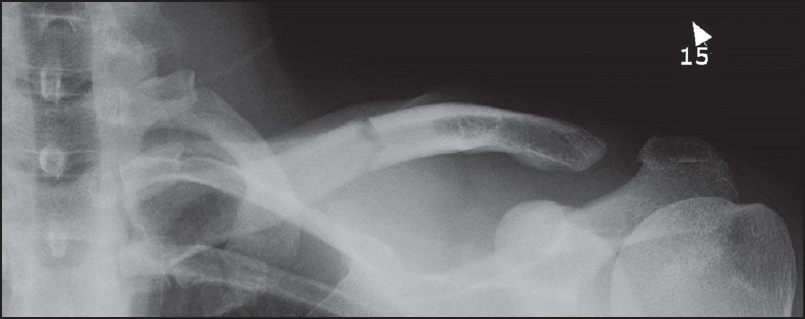  |
Type IV acromioclavicular joint dislocation associated with a mid-shaft clavicle malunion |
p. 37 |
Khalid D Mohammed, Danielle Stachiw, Alex A Malone
DOI:10.4103/0973-6042.174518 PMID:26980988This reports presents the case of a combined clavicle fracture malunion and chronic Type IV acromioclavicular (AC) joint dislocation. The patient was seen acutely in the emergency department following a mountain bike accident at which time the clavicle fracture was identified and managed conservatively however the AC dislocation was not diagnosed. The patient presented 25 months following the injury with persistent pain and disability and was treated with clavicle osteotomy and AC stabilization. We document the clinical details, surgical treatment and outcome. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
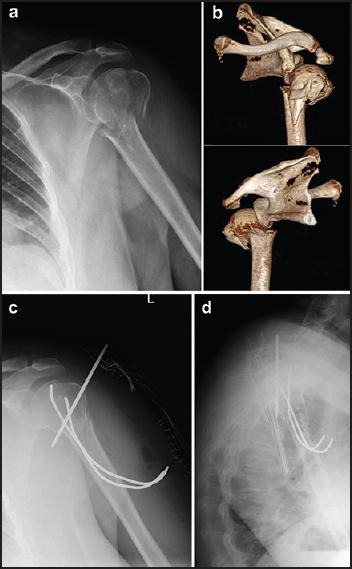  |
Early asymptomatic intrathoracic migration of a threaded pin after proximal humeral osteosynthesis |
p. 41 |
Paola Cerruti, Tony Mangano, Marcello Giovale, Ilaria Repetto
DOI:10.4103/0973-6042.174520 PMID:26980989Pinning with metallic wires is a suitable therapeutic option for proximal humeral fractures. Loosening and migration of such devices from this site is uncommon. Despite infrequently occurring, however, the literature reports dramatic and potentially lethal complications related to wires dislocation. A 69-year-old woman underwent closed reduction and fixation of a proximal 3-part humeral fracture by mean of two retrograde Kirschner wires and one anterograde threaded pin. One month after surgery, during a routine follow-up control, it was diagnosed the migration of the threaded pin in the left lung parenchyma. In the meantime, the only symptom the patient complained was an episodic intercostal pain of mild intensity, with referred onset 1 week after surgery. The migrated pin was removed through thoracoscopic approach in the emergency setting, without intra- or post-operative complications. Only a few authors reported similar complications after fixation of proximal humeral fractures. Immediate surgical removal of the device is always mandatory. When considering pinning fixation for shoulder girdle's fractures, orthopedic surgeons should take into account the risk for wire dislocation, and take up adequate precautions during surgery and follow-up control visits. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| TECHNICAL TIP |
 |
|
|
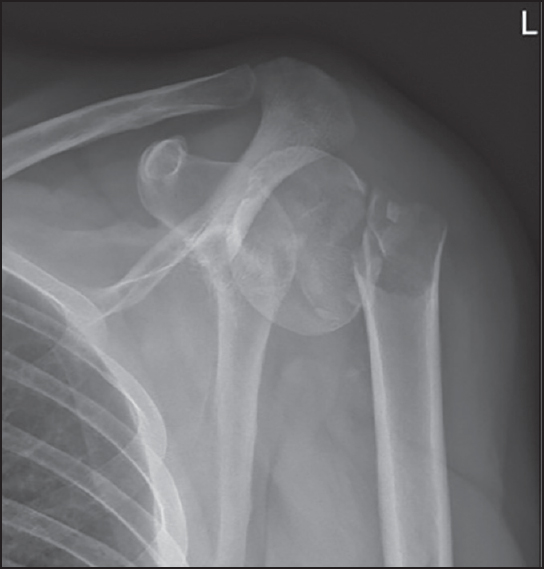  |
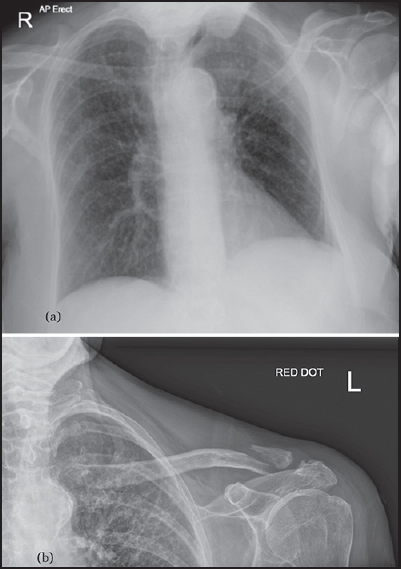
Fracture of the proximal humerus with disruption of the tendon of the pectoralis major |
p. 44 |
Bart M Berghs, Alexander Van Tongel, Thomas De Bo, Lieven F De Wilde
DOI:10.4103/0973-6042.174521 PMID:26980990Combined pectoralis major disruption and proximal humeral fractures are uncommon. A simple radiologic diagnostic tool which consists of the measurement of the displacement from the humeral shaft to the lateral side of the humeral head (lateral to the outer proximal cortex) can help to diagnose this combined lesion.
|
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| LETTERS TO THE EDITOR |
 |
|
|
  |
Snapping shoulder caused by glenoid labral bone apposition: A case report |
p. 48 |
Tomoya Takasago, Kiminori Yukata, Toshihiko Nishisho, Natsuo Yasui
DOI:10.4103/0973-6042.174522 PMID:26980991 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
A unique bipolar clavicle fracture sustained with minimal trauma |
p. 49 |
Rupert James Talboys, Mandytien Mak, Nitin Modi, Sunil Garg, Hersh Deo
DOI:10.4103/0973-6042.174524 PMID:26980992 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| ERRATA |
 |
|
|
|
Erratum: Posterior shoulder instability following anatomic total shoulder arthroplasty: A case report and review of management |
p. 52 |
DOI:10.4103/0973-6042.169803 PMID:26980993 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
Erratum: The accuracy of "subacromial grind test" in diagnosis of supraspinatus rotator cuff tears |
p. 53 |
DOI:10.4103/0973-6042.169805 PMID:26980994 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
Erratum: Long-term functional results and isokinetic strength evaluation after arthroscopic tenotomy of the long head of biceps tendon |
p. 54 |
DOI:10.4103/0973-6042.169807 PMID:26980995 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
