 |
January-June 2013
Volume 15 | Issue 1
Page Nos. 1-38
Online since Monday, September 22, 2014
Accessed 21,457 times.
PDF access policy
Journal allows immediate open access to content in HTML + PDF
|
| |
|
|
Show all abstracts Show selected abstracts Add to my list |
|
| EDITORIAL |
|
|
  |
Nigerian Journal of Surgical Research in its newest outlook as shipper of surgical scientists of the generation: Welcome! |
p. 1 |
JG Makama
DOI:10.4103/1595-1103.141380 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| ORIGINAL ARTICLES |
 |
|
|
|
Dermoid cysts of the oral cavity as seen in a Nigerian Tertiary Institution |
p. 3 |
B Fomete, BD Saheeb, EP Onyebuchi, JO Ogbeifun
DOI:10.4103/1595-1103.141381 Introduction: Dermoid cysts are rare congenital lesions derived from pluripotential cells. They represent less than 0.01% of all oral cavity cysts and are also called non-odontogenic cysts. Dermoid cysts are frequently found in sites where embryonic parts fuse together. The majority of reported cases are in the midline of the body, as well as in the ovaries and in the testicles
Patients and Methods: A retrospective analysis study that spanned the period of 2000-2012 was carried out at the Oral and Maxillofacial Surgery clinic of the Ahmadu Bello University Teaching Hospital, Zaria. The parameters studied included age, sex, duration of swelling, site, co-morbidity, complications and treatment.
Results: Of the 16 patients, 10 (62.5%) were males and 6(37.5%) females in a ratio of 1.67:1, the age ranged between 2 months and 49 years. Of all the cysts, 11 were sublingual, 3 in the cheek, 1 sublingual-submental and1 lingual; 6 (37.5%) patients had co-morbid symptoms and the most common was Upper respiratory tract infection (100%) followed by anemia (2 patients) and measles one patient.
Conclusion: Dermoid cysts can be congenital or acquired. Their early presentation were associated with both feeding and respiratory symptoms. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Sword Plugin for Repository]Beta |
|
|
|
|
|
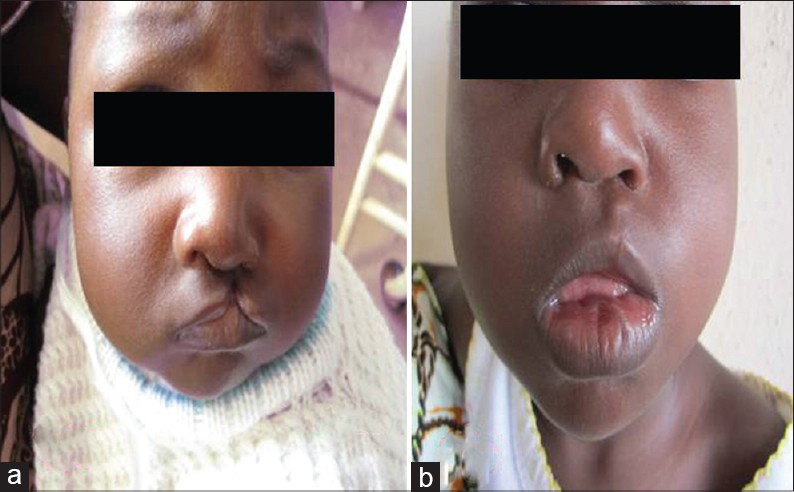  |
A Descriptive Study of Clefts of the Primary and Secondary Palate Seen in a Tertiary Institution in Nigeria |
p. 7 |
A Ibrahim, PM Mshelbwala, AC Obiadazie, CN Ononiwu, ME Asuku, SO Ajike, EA Ameh
DOI:10.4103/1595-1103.141384 Background: Cleft lip and palate is the commonest congenital malformation of the head and neck region. This article discusses the experiences of the authors' in the management of clefts of the primary and secondary palate in a tertiary institution in Nigeria.
Patients and Methods: This is a retrospective review of the clinical database for all children with cleft lip and palate. Data were analyzed for age at presentation, sex distribution, surgical technique, associated congenital anomalies, and complications. The results obtained were converted to relative values in frequency tables for analysis.
Results: The average age at presentation for all patients with cleft was 2.47 years. Males were slightly more affected than females among all clefts with a frequency of 40 (53%) and 35 (47%). The distribution of clefts by location showed a preponderance of the left side 33 (44%), followed by right side 18 (24%) and bilateral cases 11 (15%). Three patients (4%) had a relative with a cleft of the primary or secondary palate. At least one congenital malformation coexisted with a cleft of the primary or secondary palate in 13 (17%) of the 75 babies. The commonest post-operative complication of cleft of the primary palate was wound dehiscence 3 (4%).
Conclusion: This study has shown that there was a wide range of age at presentation. It is characterized by delays in the repair of clefts of the primary and secondary palate. We strongly support early repair of clefts of the primary and secondary palate to facilitate normal feeding, better speech and ensure social acceptance. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Ultrasound-guided percutaneous drainage of liver abscess: 6 years experience in Lagos State university teaching hospital, Lagos |
p. 13 |
BO Balogun, OO Olofinlade, R Igetei, CA Onyekwere
DOI:10.4103/1595-1103.141386 Introduction: Liver abscesses, both amoebic and pyogenic, continue to be an important cause of morbidity and mortality in tropical countries. The management has improved significantly over the years with the advent of potent antimicrobial agents and advances in diagnostic imaging.
Materials and Methods: From August 2007 to May 2013, 32 patients with liver abscess were referred to the Department of Radiology, Lagos University Teaching Hospital, Lagos, Nigeria for ultrasound-guided percutaneous aspiration or drainage. All patients had been treated with antibiotics or antimicrobials for at least 2 weeks before referral and were still being continued for another 6 weeks.
Results: A total of 32 patients with liver abscess were successfully treated, consisting 31 males and 1 female. The age ranged from 2 to 72 years with a mean of 43.6 years. A total of -22 (68.75%) patients had percutaneous catheter drainage, while 12 (31.25%) had percutaneous needle aspiration. A total of 15 (46.87%) patients had single abscess, while 5 (15.63%) had two and 12 (37.50%) had more than 2. Most of the abscesses are located on the right in 25 (78.12%). One needle insertion was used per patient. The amount of aspirated pus ranged from 100 to 3000 mL with a mean of 850 mL. Only 10 (31.25%) patients were on admission at the time of drainage, while the others 22 (68.75%) were day cases.
Conclusion: We found that needle aspiration and catheter drainage when combined with chemotherapy represents a successful therapeutic approach in the treatment of liver abscess whether pyogenic or amoebic. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Sword Plugin for Repository]Beta |
|
|
|
|
|
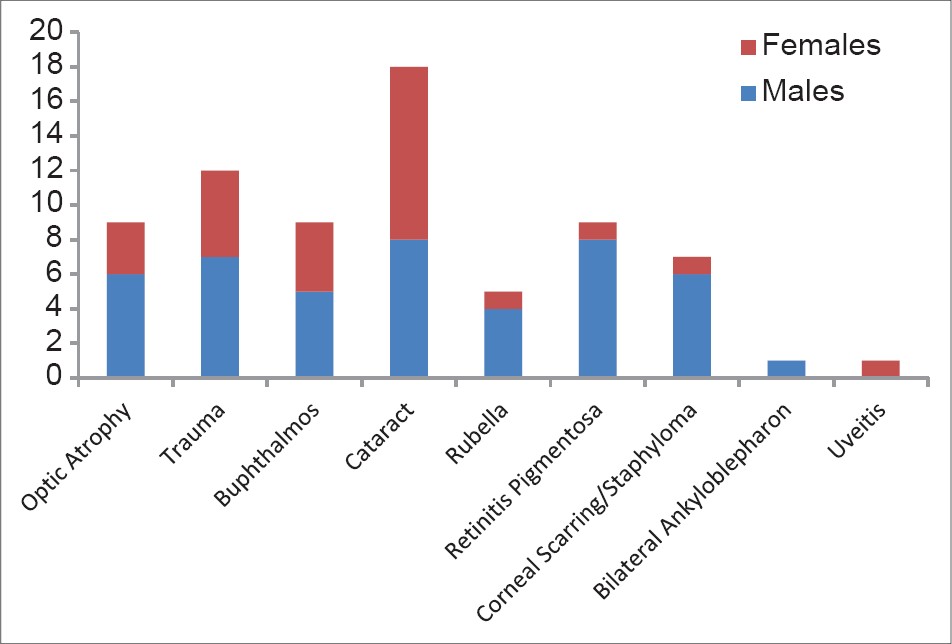  |
Causes of visual impairment and blindness in Kaduna State Special Education School |
p. 17 |
ER Abah, KK Oladigbolu, AO Ahmed
DOI:10.4103/1595-1103.141387 Aims and Objectives: To identify the causes of visual impairment and blindness in students of Kaduna State Special Education School (KASSES) and make recommendations for the planning of eye care, including prevention and management of the avoidable causes of childhood blindness in our environment.
Background: Childhood blindness is one of the priorities of vision 2020: The Right to sight. The "blind years" attributable to childhood is comparable to that of age related cataract (the commonest cause of blindness worldwide). Significant proportions of the causes of childhood blindness are avoidable and can be identified after a screening exercise and treated. Periodic screening will also provide current data for planning and implementation of childhood blindness prevention programmes.
Materials and Methods: All the students of the blind section of KASSES who were present during the study were examined and the Georgia Project's screening protocol for visual impairment in children was completed for each of them. The data was analyzed using Analyze-it V2.22 (2010) statistical software.
Results: A total of 71 students were examined. M:F ratio was 1.7:1. The age range was between 6-29 years but 76% were within the bracket of 10-19 years. Seventy percent were blind, 21% had severe visual impairment, and 9% had moderate visual impairment. Cataract was the commonest cause of blindness (25.3%), followed by trauma (16.9%), optic atrophy, buphthalmos, and retinitis pigmentosa (12.7% each). Others were corneal scarring/staphyloma (9.9%), Rubella (7.0%), and a case each of bilateral ankyloblepharon and uveitis (1.4%).
Conclusion: The causes of visual impairment in KASSES are largely avoidable. Incorporation of Primary Eye Care (PEC) into Primary Health Care (PHC) will drastically reduce needless blindness, especially in childhood and the morbidity and mortality associated with the blind years. Early identification of students with treatable causes such as cataract should also be encouraged through regular school screening and health education. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| CASE REPORTS |
 |
|
|
  |
Congenital anterior urethral diverticulum co-existing with phimosis: A case report and review of literature |
p. 22 |
A Abdulkadir, A Abubakar
DOI:10.4103/1595-1103.141389 Congenital anterior urethral diverticulum (CAUD) is a rare congenital blind ended out pouching of the urethral through the corpus spongiosium. We report its coexistence with phimosis in a 7-year-old boy who presented with difficulty in passing urine. His prepuce was not retractable and balloons at voiding. Suspected associated CAUD was confirmed at circumcision. His voiding became normal with resolution of lower urinary tract symptoms after treatment. The related literatures were reviewed. The symptoms of the two conditions mimic one another and the diagnosis of phimosis which is clinical may overshadows CAUD with its needed confirmatory imaging studies. CAUD can coexist with phimosis and high index of suspicion helps in the management. Diverticulectomy and urethroplasty with circumcision at the same sitting is curative. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Herpes labialis after scaling and root planing: Related event or non-related event |
p. 25 |
CC Azodo, P Erhabor
DOI:10.4103/1595-1103.141390 Dental treatment may trigger the reactivation and multiplication of latent herpes virus in the trigeminal nerve ganglion, manifesting as herpes labialis. However, the reported dental treatment involved the use of local anesthetic agent either in form of infiltration or block. This article reported two cases of herpes labialis in otherwise healthy 63-year-old female and 40-year-old male after non-surgical periodontal treatment without local anesthesia using ultrasonic and manual scalers, respectively. They were not bothered by the condition and did not request for any specific care. However, warm saline mouthwash, analgesics, antibiotics, and lubricating cream for the angle of mouth without antiviral prescription were recommended. In conclusion, herpes labialis may be considered a potential post scaling and root planing complication of manual and ultrasonic methods after excluding other trigger factors. Authors hereby recommend the following: 1. Minimal chairside time for scaling and employment of adequate precaution geared toward minimizing trauma to the oral mucosa during scaling among younger practitioner. 2. Inclusion of herpes labialis as a complication of scaling and root planing to reduce chances of possible litigation. 3. Prescription of preventive medications 24 hours before dental treatment and continued for two days afterwards. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Bilateral gestational gigantomastia complicated by severe sepsis; case report of a preventable mortality  |
p. 29 |
A Ibrahim, PO Enesi, PP Abur, AO Oguntayo, ES Garba
DOI:10.4103/1595-1103.141392 Gestational gigantomastia is characterized by a rapid and disproportionate growth of the breasts with a homogeneous increase in breast volume. Enlargement of the breasts with infection, ulceration and sepsis are potentially fatal for the patient and her fetus. The management is challenging, however the need for appropriate surgical intervention is rarely in question. A multidisciplinary approach regarding the decision for surgery and the timing of surgery is crucial to outcome. We report a case of gestational gigantomastia complicated by severe sepsis in a low resource setting to highlight the peculiar challenges of management. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Herniated mobile descending colon |
p. 33 |
JG Makama, P Enesi, J Jibrin
DOI:10.4103/1595-1103.141394 Persistent descending mesocolon is a congenital anomaly that has been shown, in most cases, to be asymptomatic because of its short length. To the best of our literature review and knowledge, no case of internal herniation of the mobile descending colon into either gastrocolic or splenocolic recesses have been reported. We therefore wish to report a case of herniated mobile descending colon in a middle-aged woman. HA was a 54-year-old female with a 2-year history of recurrent episodes of left upper quadrant pain of the abdomen. The pain, which was initially dull aching, suddenly became sharp in nature and so severe that it precluded her from doing her domestic activities. She had undergone clinical evaluation and work up previously but no etiology for her pain was found. After resuscitation, she consented to exploratory laparatomy for an acute on-chronic abdominal pain of unknown etiology. The intraoperative findings were a portion of the wall of the left colon seen to have herniated into a small band of tissue on the left posterior wall. The whole descending colon was unattached to the posterior peritoneum. The trapped portion (4 cm in length) of the wall of the colon was released and a warm pack was applied to the segment of large bowel so released. Following this maneuver, the portion was found to be viable and so a left colopexy was performed and the adhesion band that was placed obliquely from the spleen toward the midline was excised. Postoperative period was uneventful and since then the patient's abdominal pain has been abated over the past 1 year. The morbidity of a mobile descending colon includes internal herniation. Therefore, early detection and colopexy is necessary. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| LETTER TO EDITOR |
 |
|
|
  |
Could pfannenstiel incision for emergency caesarean section be associated with the development of uretero-vaginal fistula? |
p. 37 |
AJ Randawa, A Muhammed, L Khalid
DOI:10.4103/1595-1103.141395 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [Sword Plugin for Repository]Beta |
|
|
|
|
|