 |
January-June 2011
Volume 3 | Issue 1
Page Nos. 1-55
Online since Wednesday, March 30, 2011
Accessed 56,780 times.
PDF access policy
Full text access is free in HTML pages; however the journal allows PDF access only to users from NIGERIA, developing countries and paid subscribers.
EPub access policy
Full text in EPub is free except for the current issue. Access to the latest issue is reserved only for the paid subscribers.
|
| |
|
|
Show all abstracts Show selected abstracts Add to my list |
|
| EDITORIAL |
|
|
|
Breast conserving therapy: A surgical technique where little can mean more |
p. 1 |
Ganiyu A Rahman
DOI:10.4103/2006-8808.78459 PMID:22022642 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (4) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| COMMENTARIES |
 |
|
|
|
Laparoscopic elective colonic operation and concomitant abdominall wall hernia prosthetic repair: Safe and feasible? |
p. 5 |
Roberto Iglesias Lopes
DOI:10.4103/2006-8808.78460 PMID:22022643 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
Comment on article 'split calvarial bone graft for the reconstruction of skull defects' |
p. 7 |
Bashar Abuzayed
DOI:10.4103/2006-8808.78461 PMID:22022644 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
Spontaneous retroperitoneal hematoma: A rare devastating clinical entity of a pleiada of less common origins |
p. 8 |
Stavros I Daliakopoulos
DOI:10.4103/2006-8808.78462 PMID:22022645 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
Role of negative pressure wound therapy in healing of diabetic foot ulcers |
p. 10 |
Aziz Nather
DOI:10.4103/2006-8808.78463 PMID:22022646 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
Variations of negative pressure wound therapy |
p. 12 |
Mitsuyuki Nakayama
DOI:10.4103/2006-8808.78464 PMID:22022647 |
| [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| REVIEW ARTICLE |
 |
|
|
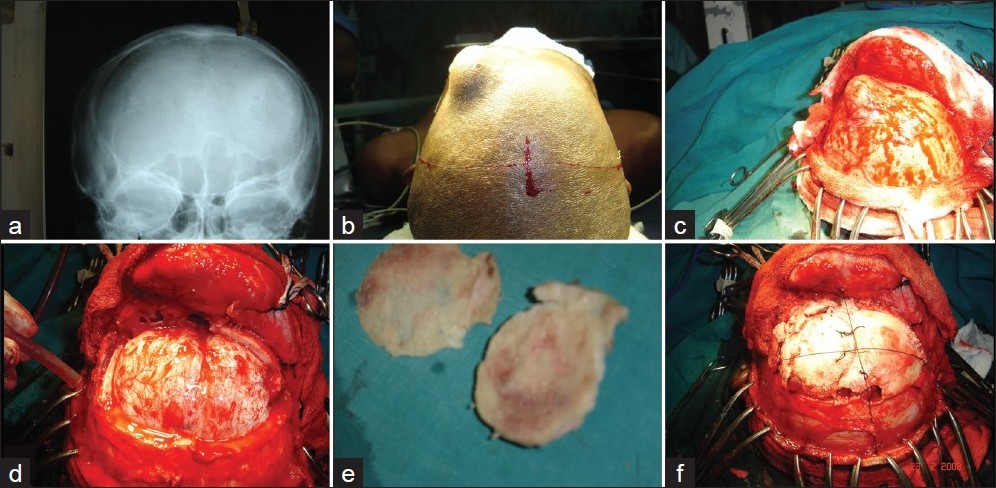  |
Split calvarial bone graft for the reconstruction of skull defects |
p. 13 |
Amit Agrawal, Lakshmi N Garg
DOI:10.4103/2006-8808.78465 PMID:22022648Cranioplasty is a common, but formidable surgical procedure for neurosurgeons, in patients with scalp and / or calvarial defects. This procedure can be simple or complex. The main objectives of cranioplasty are: To achieve primary wound healing, obliterate dead space, and seal off sterile cranial areas from contaminated oronasal cavities, to restore the normal barriers protecting the intracranial structures (together with a satisfactory cosmetic result) and obtain a permanent or very durable reconstruction, using biologically inert materials, and also to restore the aesthetics. The greatest problem is selecting the optimum material for repair of the cranial defect. Many synthetic substitutions of the dura and bone are often used for reconstruction of the skull base; unfortunately, these methods bear significant disadvantages and can induce chronic inflammation, carry a high risk of infection, and are inferior to biological sources in terms of strength and sealing quality [with the exception of some materials, such as titanium mashes and CortossTM (Orthovita® , Malvern, USA), which are seen to have more strength than the thin split thickness calvarial bone]. The primary aim of this article is to review the basic principles to use the split calvarial graft for the reconstruction of the skull defect. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (13) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| ORIGINAL ARTICLES |
 |
|
|
  |
Role of negative pressure wound therapy in healing of diabetic foot ulcers |
p. 17 |
Prabhdeep Singh Nain, Sanjeev K Uppal, Ramneesh Garg, Kuljyot Bajaj, Shirin Garg
DOI:10.4103/2006-8808.78466 PMID:22022649Introduction : Foot disorders such as ulceration, infection and gangrene are the most common, complex and costly sequelae of diabetes mellitus. [1],[2],[3] Even for the most superficial wounds, treatment is often difficult with poor healing responses and high rates of complications. The purpose of this study is to compare the rate of ulcer healing with the negative pressure dressing technique to conventional moist dressings in the treatment of diabetic foot ulcers. Materials and Methods : The study was conducted on 30 patients, which were divided into two groups. One group received negative pressure dressing while other group received conventional saline moistened gauze dressing. Results were compared for rate of wound healing. Results : There was a statistically significant difference in the rate of appearance of granulation tissue between the two groups; with granulation tissue appearing earlier in the study group. The study group promised a better outcome (80% complete responders) as compared to the control group (60% complete responders). Conclusions : Negative pressure wound therapy has a definitive role in healing of diabetic foot ulcers. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (12) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Total laryngectomy for laryngeal cancer in a Nigerian tertiary health center: Prognosis and outcome |
p. 23 |
Kufre Iseh
DOI:10.4103/2006-8808.78467 PMID:22022650Background: Advanced laryngeal cancers presenting with upper airway obstruction are a common scenario in Sub-Saharan Africa, requiring operative intervention as a priority. Objective: To assess outcome of total laryngectomy as a treatment option in the surgical management of advanced laryngeal cancers in a tertiary health institution in northwestern Nigeria. Materials and Methods: A retrospective analysis of total laryngectomies for laryngeal cancers carried out by one surgeon from December 2000 to August 2009. Results: Out of 30 patients with histologically diagnosed laryngeal cancer, 18 were treated with total laryngectomy Fourteen (77.8%) were males, while 4 (22.2%) were females, with a male-to-female ratio of 3.5:1. The age range was 20-70 years with a mean age of 47years for males and 33.8 years for females. Total laryngectomy was carried out on T4 lesions (100%), with preoperative tracheostomy (100%) carried out as an emergency measure to relieve upper airway obstruction. Two female patients had safe vaginal deliveries after their surgeries. Although all patients were referred for radiotherapy, only 6 (33.3%) patients could afford postoperative radiotherapy, with a 5-year survival rate of 33.3%; while all others could not afford the cost of radiotherapy treatment, which was to be carried out at a center about 5 hours drive away from our center. Seven (38.9%) patients presented with recurrent neck nodal disease, while 3 (16.7%) had carotid blow-out hemorrhage that was fatal. Conclusion: Total laryngectomy remains an important surgical modality of treatment for advanced laryngeal cancers, as it affords the patient an opportunity of longer survival when combined with postoperative radiotherapy. It is superior to 'radiotherapy only' or 'surgery only' or nothing. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
|
| CASE REPORTS |
 |
|
|
  |
Anastomosis procedure through an inguinal hernia incision in simultaneous laparoscopic anterior resection and inguinal hernia repair |
p. 31 |
Toshimasa Suzuki, Hidejiro Kawahara, Naoko Iida, Masaru Naruse, Takeyuki Misawa, Katsuhiko Yanaga
DOI:10.4103/2006-8808.78468 PMID:22022651For laparoscopic anterior resection, an additional small incision is usually placed in the left lower quadrant or the suprapubic portion. As a left inguinal hernia incision is close to both the left lower quadrant and the suprapubic portion, such an incision can be used for anastomosis in laparoscopic anterior resection, without additional incisions. We report a laparoscopic anterior resection using a left inguinal hernia incision for colorectal anastomosis, in a patient who underwent concomitant left inguinal hernia repair. After a total mesorectal excision was performed laparoscopically, the distal portion of the rectum was transected by a stapler. A 4 cm skin incision was made in the left inguinal region and carried down to the peritoneum through the hernia sac. The bowel resection was performed extracorporeally, and an anvil was placed at the proximal end of the colon over a purse-string suture. After colorectal anastomosis was performed using a circular stapler inserted through the anus, the inguinal hernia was repaired with a mesh. The inguinal wound healed without surgical site infection, and the patient was discharged ten days after surgery. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
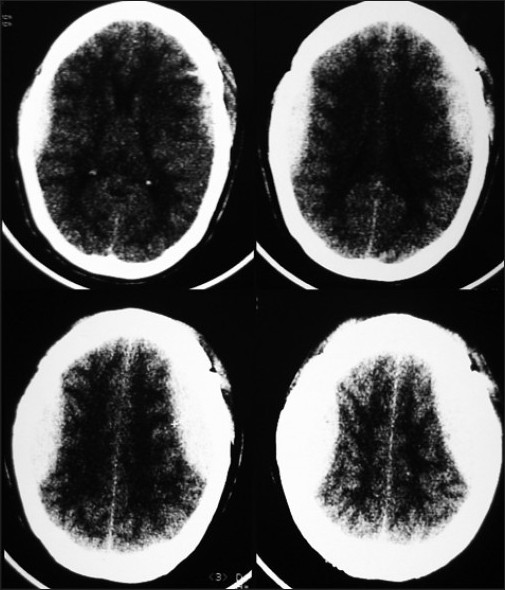  |
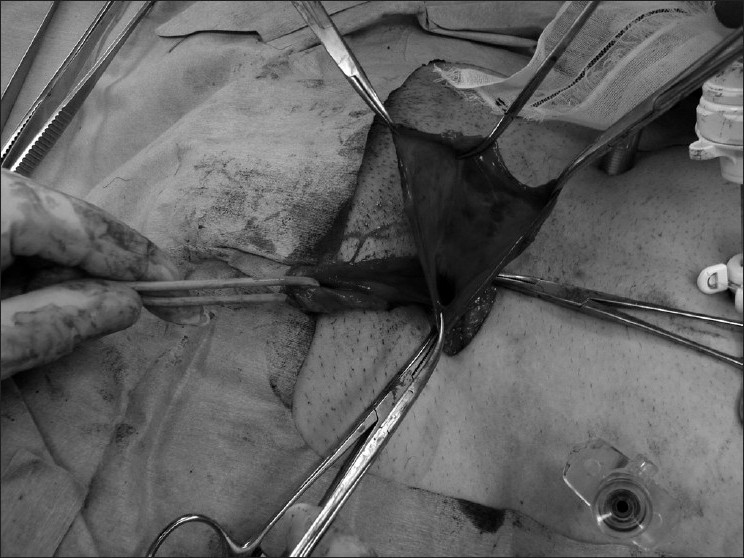
Bilateral symmetrical parietal extradural hematoma |
p. 34 |
Amit Agrawal
DOI:10.4103/2006-8808.78469 PMID:22022652The occurrence of bilateral extradural hematomas (EDH) is an uncommon consequence of craniocerebral trauma, and acute symmetrical bilateral epidural hematomas are extremely rare. We discuss the technique adopted by us for the management of this rare entity. A 55-year-old patient presented with history of fall of branch of tree on her head. She had loss of consciousness since then and had multiple episodes of vomiting. Examination of the scalp was suggestive of diffuse subgaleal hematoma. Her Glasgow coma scale was nine and there were no lateralizing signs. Her computed tomography scan showed bilateral, symmetrical, parietal EDH with diastases of coronal suture. The patient underwent bicoronal scalp flap well behind the coronal suture running across the junction of anterior two-third and posterior one-third of hematoma to gain bilateral exposure. Initially, left parietal trephine craniotomy was performed and without disturbing the blood clot, left trephine craniotomy was performed and the hematomas were evacuated. Management of bilateral EDH cases requires careful planning, adequate exposure, judicious surgical approach, and time management for good results. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (2) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Penile gangrene: An unusual complication of priapism in a patient with bladder carcinoma  |
p. 37 |
Abdulwahab A Ajape, Ahmad Bello
DOI:10.4103/2006-8808.78470 PMID:22022653A 40-year-old, apparently healthy farmer presented with a 4-day history of progressively painful penile erection with no known predisposing or precipitating factor. He had an emergency El-Ghorab shunt which resulted in almost complete detumescence. He was noticed to have developed ischemic changes of the distal part of the penile skin which progressed to gangrene of the distal part of the penis on the 4th day post intervention. Abdomino-pelvic ultrasound revealed an intravesical mass and urine and corpus cavernosa aspiration cytology were positive for malignant cell. The patient, however, declined further treatment and was discharged against medical advice. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (8) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Traumatic fracture of thin pedicles secondary to extradural meningeal cyst |
p. 40 |
Daniel S Yanni, Antonios Mammis, Nikhil G Thaker, Ira M Goldstein
DOI:10.4103/2006-8808.78472 PMID:22022654Spinal dural meningoceles and diverticula are meningeal cysts that have a myriad of clinical presentations and sequelae, secondary to local mass effect. Our objective is to report a technical case report, illustrating a traumatic spinal injury with multiple pedicle fractures, secondary to atrophic lumbar pedicles as well as the diagnostic workup and surgical management of this problem. Posterior lumbar decompression, resection of the meningeal cyst, ligation of the cyst ostium, instrumentation, and fusion were performed with the assistance of intraoperative isocentric fluoroscopy. The cyst's point of communication was successfully located with intraoperative fluoroscopy and the lesion was successfully excised. We suggest that patients with traumatic spinal injuries, having evidence of pre-existing anomalous bony architecture, undergo advanced imaging studies, to rule out intraspinal pathology. The positive clinical and radiographic results support the removal and closure of the pre-existing meningeal cyst at the time of treatment of traumatic spinal injury. Intraoperative isocentric fluoroscopy is a helpful tool in the operative management of these lesions. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
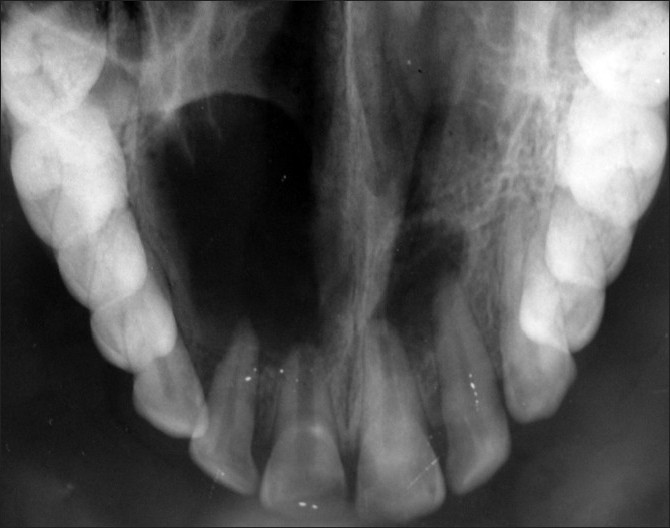  |
Surgical and nonsurgical management of bilateral periapical lesions in the maxillary anterior region |
p. 44 |
Sweta Tolasaria, Utpal K Das
DOI:10.4103/2006-8808.78473 PMID:22022655Conventional nonsurgical endodontic treatment has a high degree of clinical success, but in certain cases surgical intervention becomes necessary. This is the case report of a patient presenting with bilaterally separate periapical lesions in the maxillary anterior region. One lesion was managed by periapical surgery using a novel and safe method of separating the soft tissue mass of the periapical lesion which was in proximity to vital and vulnerable anatomical tissues, and the other was managed by long-term intracanal medicament, emphasizing the need of application of treatment in the best interest of the patient. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
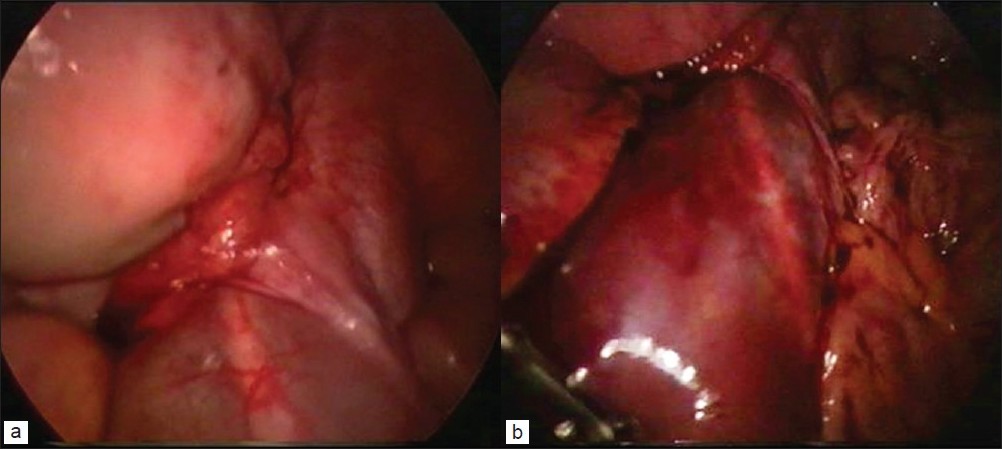  |
Idiopathic retroperitoneal hematoma |
p. 49 |
Sherif Monib, Andrew Ritchie, Ezzuldin Thabet
DOI:10.4103/2006-8808.78475 PMID:22022656Idiopathic retroperitoneal hematoma is a rare, but potentially life threatening cause of an acute surgical abdomen. Initially diagnosis may be overlooked, leading to unnecessary exploration, which may have implications for prognosis of the patient. An enhanced Computer Tomography (CT) scan of the abdomen is the principle method of diagnosis. However, as in our case, laparoscopic management of the acute abdomen can play a vital role in this group of patients. Importantly, early diagnosis and vigilant conservative management can improve the outcome in idiopathic retroperitoneal hematoma. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (4) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|
  |
Management of maternofetal emergency in shock with fracture of femur |
p. 52 |
Pradeep K Singh, Deepti Shrivastva, Snigdha Paddalwar, Nagraj Shetty, Vipin Raut, Sarthak Patnaik, Abhishek Yadav
DOI:10.4103/2006-8808.78477 PMID:22022657Trauma is the leading nonobstetric cause of maternal death. The worst complication can be fetal compromise that threatens premature labor or even fetal death. We are reporting a case of a 30-year-old primi, short stature woman who had fracture femur with hypovolaemic shock. Managing such trauma complicated by shock in a pregnant patient needs multidisciplinary approach. Clinician team evaluating and coordinating the care of pregnant trauma patient should understand the pathophysiological changes in pregnancy with trauma to manage hypovolaemic shock, related complications, treatment of fracture, and radiation exposure to the fetus. The use of imaging studies, invasive hemodynamics and surgery, if necessary, should be individualized. A clear understanding of fetal viability, physiological changes of pregnancy, and pathophysiology of shock, is mandatory for optimal, maternal functional, and obstetrical outcome. |
| [ABSTRACT] [HTML Full text] [PDF] [Mobile Full text] [EPub] [Citations (1) ] [PubMed] [Sword Plugin for Repository]Beta |
|
|
|
|
|